Quick Reference Guide
for
FFM D Applications
Table of Contents
-1-
Federal Facilitated Exchange (FFE)/”Marketplace” and FFM D Cases
The FFE and Marketplace are synonymous terms. In this desk tool we will use the term “Marketplace” when speaking about FFM D cases. Virginia uses the Federally Facilitated Marketplace (FFM) while some other states have their own Health Insurance Marketplace (HIM). Initially, the Marketplace only forwarded potentially Medicaid eligible health insurance applicants to the Commonwealth via VaCMS as FFM Referrals for eligibility determination.
Beginning in November of 2018 the “Marketplace” equipped with the Virginia Medicaid guidance and policies began to determine Medicaid eligibility for submitted health insurance applicants. These cases were forwarded to VaCMS, landing in My Workspace (MWS) with a Source Type identifier of FFM D. The FFM D identifier indicates that the “Marketplace” using Virginia rules has already ran and completed an eligibility determination.
The “Marketplace” only interfaces with VaCMS in the transferring of applications/cases to VaCMS MWS. Therefore, the “Marketplace” does not know about existing applications and/or approved cases for individuals submitting applications to the “Marketplace”.
-2-
Overview of Processing FFM D Cases
The assignment of 'Processing Unit' in MWS for FFM D cases is the same as referrals from the FFM.
We have intentionally used the term “cases” in reference to FFM Ds that land in MWS, specifically because the eligibility determination has already been completed by the Marketplace. Even when the Processing Status is 'New” in MWS the Marketplace has determined eligibility, however, there was a failure in VaCMS for the case.
Eligibility Workers and staff working in MWS should be aware of:
The FFM D identifiers in MWS
The different processing statuses associated with FFM D cases
The alerts generated for FFM D cases
Business Processes specific to FFM D cases
Decisions made related to the “Known to VaCMS” processing status:
When FFM D cases began landing in MWS the process was failing the majority of the cases.
Customers were applying at the Marketplace, including for children who were currently receiving MA, causing cases to fail.
It was requested to modify the coding so that more of the Marketplace cases would no longer fail.
It was recommended that the associating of FFM D cases not take place (understanding this would cause duplicate cases) a search would be done in VaCMS to ensure the same client ID would be assigned, and the same MMIS enrollee ID (this prevents duplicate MA Cards/enrollees)
Another occurrence that is seen is customers applying multiple times (2 or more times). When customers have applied with the Marketplace multiple times, these applications will display in MWS with the processing status of “Known to VaCMS”.
The next several pages will speak to these bulleted items.
-3-
FFM D Identifiers and My Workspace (MWS)
FFM cases that land in MWS will have an indicator(s) in the Source Column meant to let the worker know that:
eligibility has been determined (D)
the application is being referred for determination; the default will receive an alert (R)
the case has a combination of individuals; some for whom eligibility has been determined and
some for whom eligibility must be determined; an alert will be presented to the default worker identifying the individuals for whom eligibility must be determined (R&D)
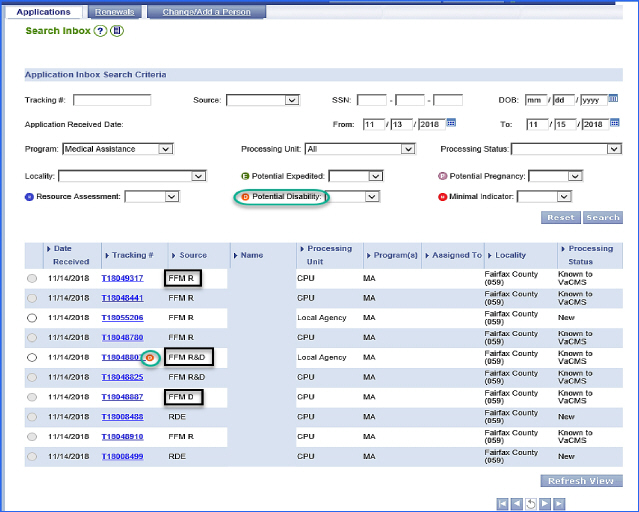
The screen capture below displays the different FFM identifiers in the Source Column. We also
want to point out
that a new element will also display in the Tracking
Number Column. The ![]()
displays in the Tracking Number Column is different from the FFM identifiers in the Source
Column; this ![]() lets the worker know
that a YES response to the disability question has been
lets the worker know
that a YES response to the disability question has been
selected for a person on the application.
-4-
Marketplace applications that land in MWS with FFM D in the Source column can have a number of different Processing Statuses in MWS. The Processing Status guides the worker to the next steps.
Below is a list of the Processing Statuses as related to the cases in MWS with FFM D in the Source column.
FFM D |
Action |
New |
Ordinarily,
this status will NOT display with “FFM
D”. However when the 'Processing |
Started |
These cases
failed during the file clearance process. |
Known to |
This processing
status is assigned when at least one individual on the application
submitted |
Continue Case |
This processing
status is assigned when an individual(s) on the application submitted
to the |
FFM-Different |
This processing
status is assigned when the application submitted to the Market
place has |
Submit |
This processing
status will be assigned to applications from the Marketplace,
landing in
|
-5-
FFM D Generated Task and Reminders (Alerts)
Task and Reminders
(alerts) are generated for FFM D
cases, based on the ![]()
![]()
Processing Status and provides guidance to workers as to steps the workers
may need to take.

Workers should access Task and Reminders using either T#s or the case # prior to moving forward to process a FFM D case.
Alerts may be generated for FFM D cases with processing statuses in MWS of:
New
Started
Submitted
Continue Case Assignment
Processing Statuses of New and Started:
FFM Determination failed at “File Clearance”.
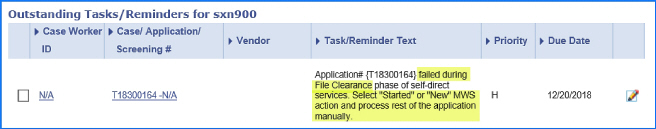
Workers will access MWS at the radio button
for “New” statuses and the hyperlink
for “Started” statuses to continue File Clearance.
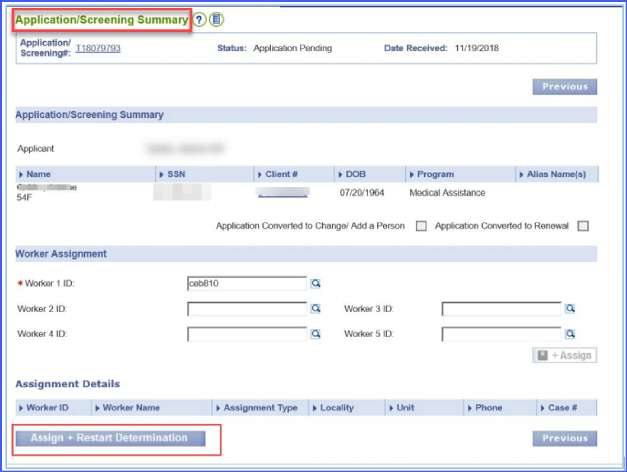
Complete the case from “File Clearance and on the Application/Screening
Summary screen be sure to select the “Assign
+ Restart Determination” button. The
Case should continue the case through certification.
Processing Status of Submitted (there are several Task/Reminders for this status):
FFM Determination has completed.
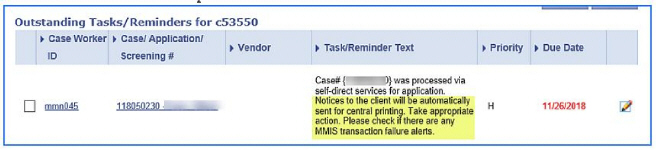
When the above alert is received, workers should ensure that all MMIS transactions were successful and that a notice is in Forms History.
-6-
FFM Determination has completed.

When the above alert is received, workers
should evaluate impact, if any, on other active programs such as SNAP
or TANF.
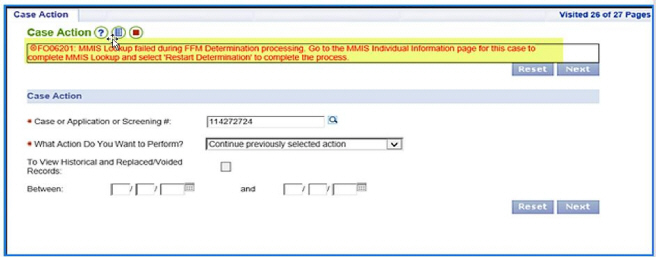
FFM Determination
has completed Data
Collection, however,
there is a failure during MMIS Look
up.
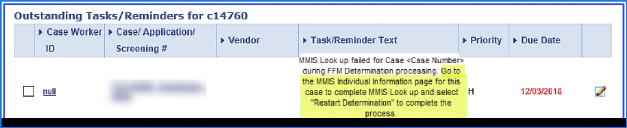
When the above alert is received, workers
will need to access 'Eligibility Summary' from the VaCMS Left Nav and proceed to MMIS
Individual Information page to resolve failures.
Processing Status of Continue Case Assignment
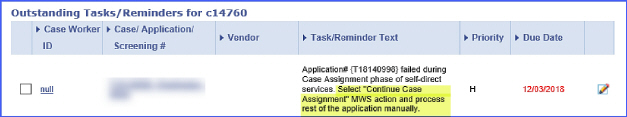
When the above alert is received, workers
will need to access MWS, select the “Continue Case Assignment” hyperlink
and on the Application/Screening Summary
screen assign a worker and select the “Assign + Restart Determination”
button.
-7-
FFM D Cases - - Before Getting Started
Before Getting Started with Processing FFM D Cases
When encountering FFM D cases, eligibility workers and staff should be aware of the following important processes.
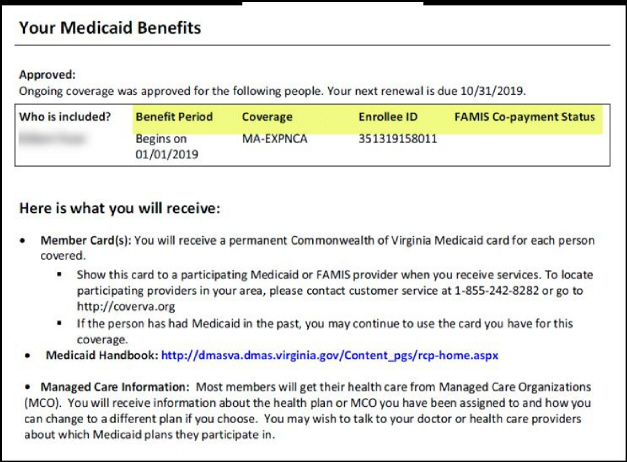
Eligibility has already been determined for FFM D cases. VaCMS maps “Marketplace” determinations to the appropriate Aid Category.
CPU/LDSS running eligibility will override the Marketplace determination.
«At times, such as when FFM D does not complete data collection you may need to run eligibility to complete the case.
(See sample Marketplace letter below).
|
-8- |
Workers should view alerts associated with the Tnumber and/or Case Number: alerts provide guidance as to current status of the case and next steps for the worker.
Complete inquiries on every person on the application before you get started to be sure you will be able to complete the action prior to initiating the FFM D case; i.e., as a pending application.
When there is an existing VaCMS case(s) be sure to associate to the correct case.
-9-
Individual Currently Enrolled Full Coverage:
Eligibility Current- deny FFM-D using Application Disposition as a duplicate application
Case Narrative Language for Duplicate Applications:
FFM determinations (T#) received on xxxx Applicant currently already enrolled as full benefit Medicaid recipient. FFE application denied as duplicate.
§ This is to be followed by your LDAP
Renewal Due TBD (information to be provided)
Individual Enrolled in Limited Coverage:
Eligibility Current- convert FFM-D using case association to a change, update 'Data Collection' with the information received from the FFM and then run eligibility:
§ No verification checklists are to be generated because eligibility has been
determined by the FFM.
§ 'Other' should be selected as the verification source and documented that the
verification was completed at the Marketplace.
§ Since you have to run eligibility, make sure to put the following language
in the case narrative: “The case was determined eligible by FFE. Per Federal guidance the State is not to rework eligibility.” This is to be followed by your LDAP.
Renewal Due TBD (information to be provided)
Individual has multiple applications filed or pending for MA-
If the other applications have not been associated to the customer's existing case complete the case association, assign and restart the determination for the FFM-D
If another application has already been associated to the case or is pending, hold the FFM D until a disposition of the pending application is completed.
§ Approved Full Coverage
If the individual is determined eligible for full coverage then deny the FFM D in 'Application Screening'.
-10-
§ Approved Limited Coverage
If the individual was determined ineligible for full coverage follow the steps above for the individual enrolled in limited coverage with current eligibility.
§ Denials
If the individual is denied but others on the case are approved convert the FFM D to a Change/Add a Person to process through 'Data Collection'.
r No verification checklists are to be generated because eligibility
has been determined by the FFM.
r 'Other' should be selected as the verification source and
documented that the verification was completed at the Marketplace.
Since you have to run eligibility, make sure to put the following language in the case narrative:
“The case was determined eligible by FFE. Per Federal guidance the State is not to rework eligibility.” This is to be followed by your LDAP. If the case is denied complete case association for the held FFM D case and attempt to restart the automated processing. If the automated processing is not successful complete steps for FFM D cases for which eligibility must be ran.
If the individual has an application pending for another program (SNAP or TANF) which is preventing case association, the agency should determine if everything is available to process the pending case that day to complete case association.
§ If the case cannot be completed that day then use the QRG for Adding a
Program to a Pending Case or wait until the pending action is completed to use the automated processing of the FFM D.
§ If the worker must run eligibility to complete the FFM D transfer to 'Data
Collection' in VaCMS remember:
No verification checklists are to be generated because eligibility has been determined by the FFM.
'Other' should be selected as the verification source and documented that the verification was completed at the Marketplace.
Since you have to run eligibility, make sure to put the following language in the case narrative:
“The case was determined eligible by FFE. Per Federal guidance the State is not to rework eligibility.” This is to be followed by your LDAP.
-11-
Screen Captures of Beginning to End Processes
Processing a FFM D Case with Processing Status of Submitted with no existing case numbers.
Access My Workspace (MWS) from the Left Nav. Select FFM D application with Processing Status of “Submitted”.

Next, access “Inquiry” from the Left Nav to see if there are established case numbers for the MWS Tnumber.
this step you want to be sure the correct
case number is attached to the FFM
D application.
-12-
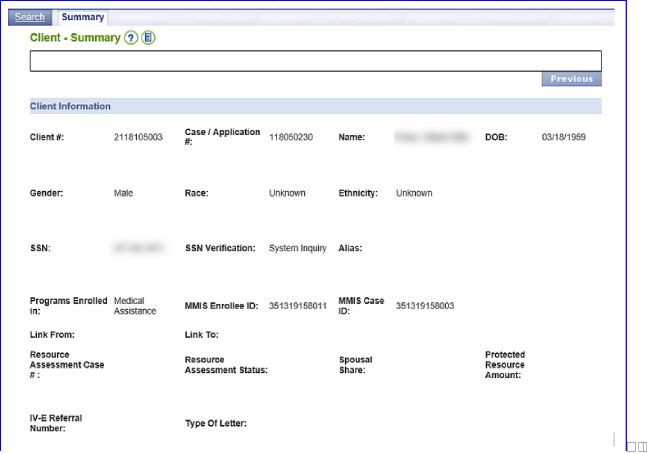
Compare the FFM D Application Information, Referral Details to the individuals on the VaCMS case for accuracy.
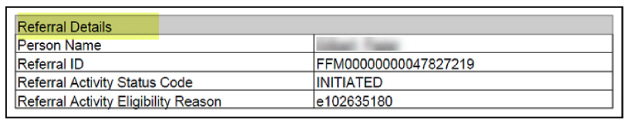
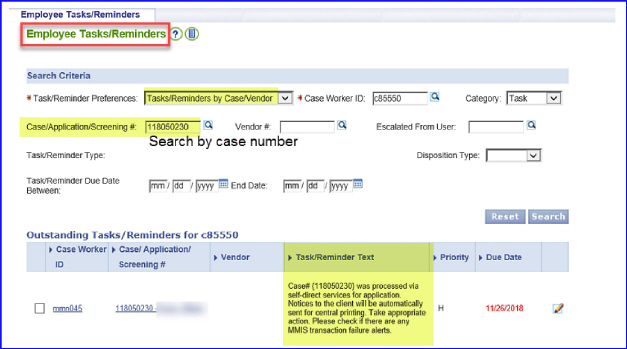
«For each FFM D application an alert (Task and Reminder) is generated. The alert guides the worker as to the action needed. From the Left Nav, select Dashboard Tools then Task and Reminders.
This alert tells the worker that eligibility determination has been completed (case has been authorized and certified) and notices have been generated. Review the case to validate there are no MMIS failures.
-13-
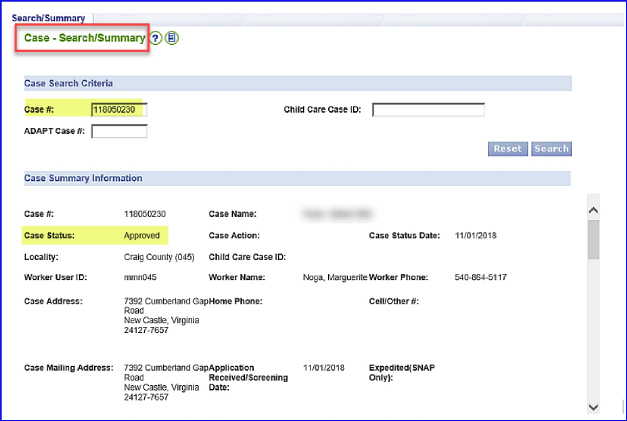
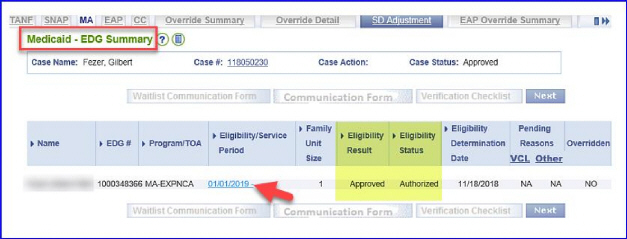
Validate case status displays as “Approved” and individuals are enrolled in MMIS.

-14-
From the Left Nav,
select Eligibility Search to validate EDG information. Select the
hyperlink.
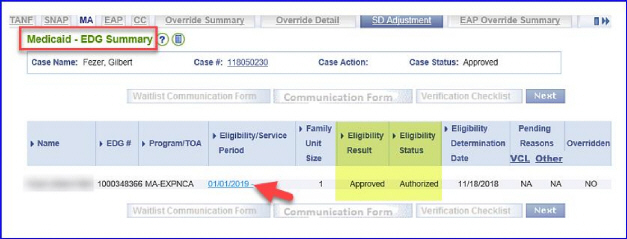
The Medicaid Eligibility EDG Summary screen will display. On this screen select the FFM Determination tab to see FFM information.

-15-
The Medicaid Eligibility FFM Determination screen will display. On this screen you will see the information sent by the Marketplace to VaCMS.
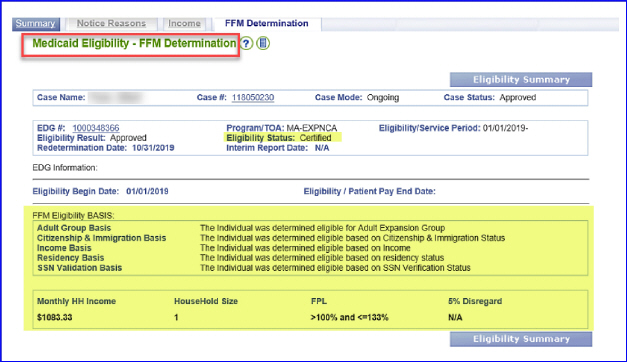
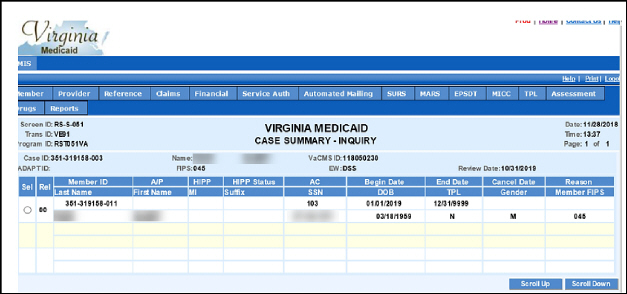
Now, access MMIS to validate successful enrollment.
-16-
Now, validate that the correct notice was generated.
-17-
Processing a FFM D Case with Processing Status of Continue Case Assignment
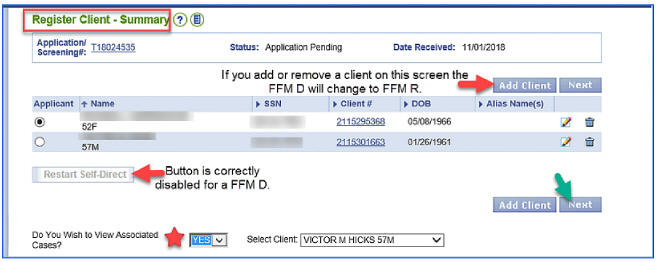
NOTE: Names and SSNs have been blurred out when test data not used.
The Continue Case Assignment processing status is assigned when individuals on the application submitted to the Marketplace are known on at least one VaCMS case and the current applicant is not the VaCMS case name.
To process a FFM D case, access VaCMS and My Workspace. Select the hyperlink in the Processing Status column. If the link is unavailable go to Maintain Application Screening, enter the T# then select the edit button to continue the file clearance and case association.
« The individuals' name listed in the Name column is the name of the individual that submitted the Marketplace application but you have to review the PDF to determine the applicants. Reviewing existing FFM Help documents in VaCMS can provide additional information.

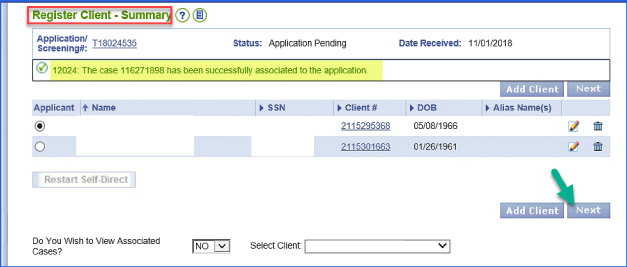
The Register Client Summary screen will display. The worker should select YES at the 'Do you wish to view associated cases' question. This is necessary to prevent the creation of multiple case numbers for an individual.
-18-
The File Clearance Associated Cases screen will display. Cases and applications will display. The worker must access each case/Tnumber to determine which case the current Marketplace applicant is the Case name in VaCMS.
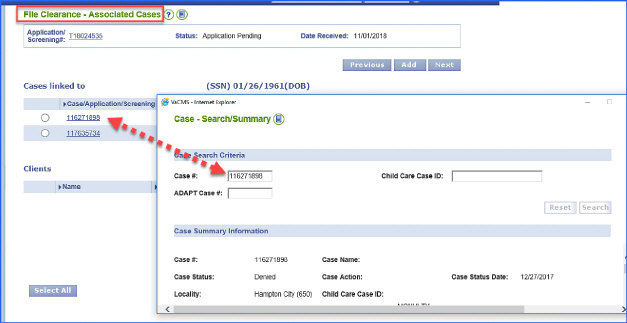
-19-
After identifying the VaCMS case where the Marketplace applicant and VaCMS case name match select that case on the File Clearance Associated Cases screen.
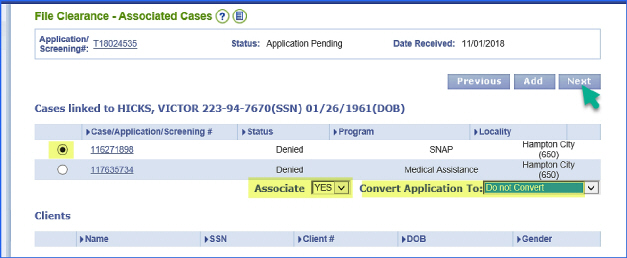
The appropriate message will display. «If you do not get this message STOP - - - the case has not been associated. Continuing will cause a duplicate case to be created.
-20-
The Register Program Program screen will display. On this screen you will select the “Save + Continue” button, unless a change is required at the bottom section of the screen.
Note changing anything on this screen will change the FFM-D application to an FFM-R application in MWS and how the application must be processed.
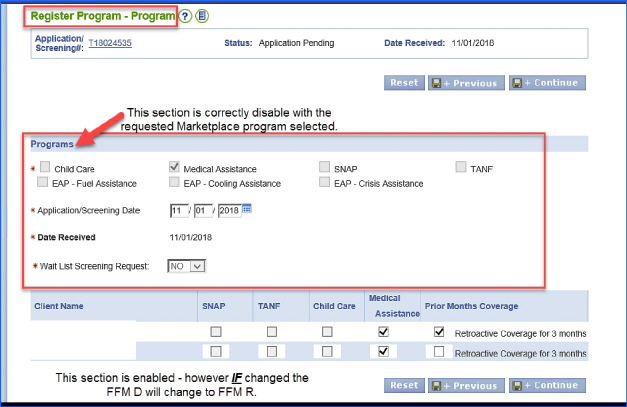
The Application/Screening Summary screen will display, enter you as the assigned worker then select Assign & Restart Determination.
-21-
This application will process via Self-direct. The Tnumber will not be searchable in MWS. (While SD is running no one else should touch the case that is why it is temporarily hidden from view)
After File Clearance has run, check “My Tasks and Reminders” for an alert. Follow the guidance in the alert for next steps. Reminder: When a Task and Reminder says “process manually”, remember you are to select the “Assign + Restart Determination” button.
-22-
Business Processes after Selection of the 'Assign + Restart Determination' Button
The Processing Status will now display as 'Submitted', however, processing is not successful through authorization.
Check Task and Reminders for alerts to determine why and where the application failed in processing
If the case has an alert that states the case fail during the “Data Collection” process finish updating the case details and then run eligibility:
§ No verification checklists are to be generated because eligibility has been
determined by the FFM.
§ 'Other' should be selected as the verification source and documented that the
verification was completed at the Marketplace.
§ If we have to run eligibility, make sure to put the following language in
the case narrative: “The application was determined eligible by FFE. Per Federal guidance the State is not to rework eligibility.” This is to be followed by your LDAP.
If the case has an alert that states the case failed during the “Eligibility
Determination” process:
§ Go to “Eligibility Summary” and review the EDG for the individuals that were
evaluated for eligibility.
-23-
§ If you see an FFM Determiniation tab go back to Eligibility Summary.

§ Then click “Next” you should be directed to the MMIS Individual Detail
Screen
Complete the MMIS Individual Detail Look-up
Then select the Restart Determination Button
§ Check to see if MMIS transactions and authorization were successful. Notices
should be in pending forms.
Note if these steps are not successful attempt to complete the case by continuing the case action and use the documentation provided for FFM-D applications that had eligibility ran to complete the case.
-24-